[Reposted with permission from the website of Dr. Richard Kellogg (where details of his analysis techniques can be found) a physicist at the Conseil Européen pour la Recherche Nucléaire (CERN). At NWCitizen we find that his piece has information that is very helpful in understanding the nature of the COVID-19 pandemic. We are grateful to Dr. Kellogg for allowing us to share his insights with us.]
We are faced with a novel viral enemy against which the global human population has no immunity. This enemy attacks us in its own peculiar manner, being highly contagious, producing light symptoms in many of its victims, so that they continue their usual activities while spreading their infection, but attacking others, mostly the old, much more aggressively, to the point of fatality.
Studying the early spread of COVID-19 in the West, before policies of social isolation were adopted to slow the progression of the disease, the value of R0, the number of new infections produced by each carrier of the disease was found to be about 4. In China, the disease was tamed by introducing very strict quarantine which reduced R0 to less than unity. Thus deprived of growth, the epidemic in China died away to the point where no new infections were observed, and after 3 months, the quarantine was able to be lifted after less than 10^-4 of the population had been infected.
In the West, the rigorous Chinese quarantine measures have been considered impractical, and most countries have settled on various degrees of more modest social isolation measures. These have nevertheless led to serious disruption of normal life, but have not managed to reduce R0 below 1.1 to 1.5. This has certainly slowed the growth of the contagion, but not stopped it, let alone snuffed it out. Assuming that people who become infected either recover and acquire immunity, or die; if these R0 values can be maintained, the contagion will ultimately reach a saturation level, Sf, the fraction of the population which has been infected:
Sf = 1 - 1/R0
So the smaller the R0, the smaller will be the ultimate fraction of people infected. If R0=1.00, Sf=0. If R0=2, Sf=0.5. But the smaller the R0, the longer it takes to approach saturation. To get approximately to 90% of ultimate saturation, it takes:
T_90 = 25 days/log_10(R0)
So for R0 = 2, T_90 = 80 days, for R0 = 1.50, T_90 = 140 days. For R0 = 1.1, T_90 = 600 days. Maintaining current isolation conditions for 6 months or more poses a challenge, but worse, if R0 is not brought to less than 1.00, then there will always remain a small number of carriers in the population, no matter how long one waits. As soon as the isolation measures are relaxed, the contagion will start to grow again from those seeds. There are only four basic ways to exit the COVID-19 epidemic, which I list in order of desirability:
1. Invent an effective vaccine, and vaccinate everyone
2. Allow the contagion to run its course under normal social conditions, in which case the disease ultimately becomes endemic, with a steady, low level of new infections
3. Reduce R0 below unity, and follow the Chinese example
4. Limit R0 through social isolation measures for long enough
that the number of carriers becomes small enough that they can all be traced
and isolated from the general population until they either recover or die
Option (1) is obviously best. All we need is to bell the cat. But estimates of the time needed to develop, test, and deploy an effective vaccine range from a year to 18 months. What should we do in the meantime?
Option (2) is the one traditionally taken. For most of human history, it was the only available option. It results in a population with “herd immunity” so society is inherently safe, although many lives will be lost in the epidemic phase, and isolated deaths will occur at a low rate thereafter. Taking R0 = 2 and a fatality rate of 1%, 0.5% of the population will die within a few months in the epidemic phase. Most of the deaths will hit people older than 70.
Both Options (3) and (4) leave a large fraction of the population unexposed to the virus, and therefore susceptible to a re-ignition of the epidemic if even a single carrier either is left unfound, or arrives from a foreign destination. I would note that South Korea was successful with a special version of Option (4), by rigorously applying it before their epidemic had a chance to grow appreciably.
An additional problem with Option (2) is that the rate of infections during the epidemic phase will certainly overwhelm any national healthcare system, resulting in a higher fatality rate, and untold human suffering.
Currently no Western country has managed to pursue Option (3), in fact most countries talk about relaxing their current isolation measures, due to the toll they are taking on their economies. There would appear, therefore, no practical alternative other than to pursue a modified Option (4) while we wait for an effective vaccine, gradually relaxing isolation measures at a rate which pushes the healthcare system to its limit, but not beyond.
From current experience in NYC it is likely that the US, with R0 = 1.5 is at, or somewhat above the level of health system overload. Since in the U.S. only about 1% of the population has yet been infected and the number of deaths is increasing by a factor of 10 every ~18 days, it will be about 3 weeks before we can expect to approach saturation to the point social isolation measures can be loosened without overloading health care. Since the U.S. is a big country, the timing of relaxation will vary considerably, depending on locality.
The optimal point to begin relaxation is when about 15% of the local population has been infected, and it will certainly be a challenge to choreograph the relaxation in time and place while an additional 35% of the population suffers the disease. If this relaxation could be managed perfectly, the healthcare system would continue to work at its emergency level for another 2 months. But since fine-tuning such social engineering at that level will be virtually impossible, it is likely to be well into Fall before the epidemic phase is over, and one can attack the remaining carriers through tracing and isolation.
Assuming this scenario, 0.5% of the U.S. population will have died of COVID-19 by September, representing 1.7M deaths. Without COVID-19, 2.6M Americans die every year. I have compared the annual U.S. non-COVID-19 mortality by age with the expected mortality due to coronavirus if the epidemic is allowed to proceed to saturation under normal social conditions (R0=2.0, saturation =0.5):
Here are the essential results:
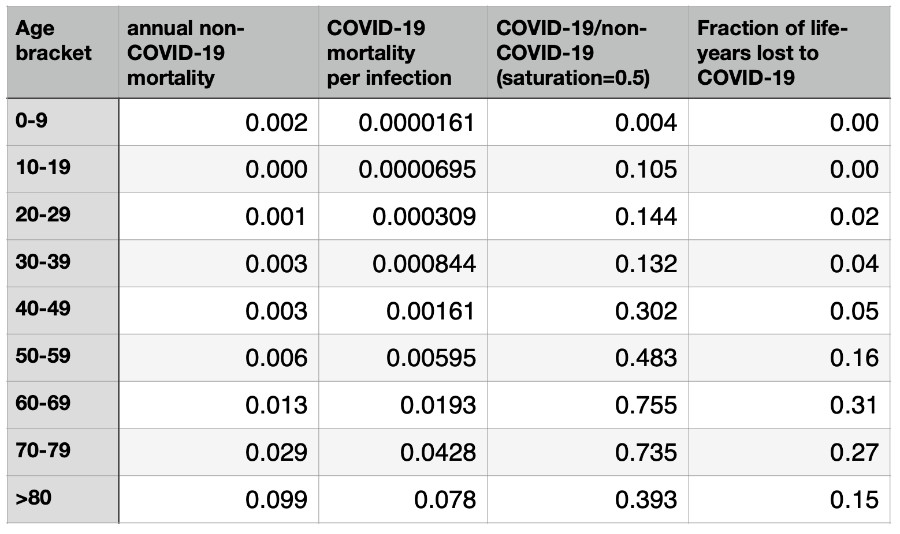
Even in the age brackets most likely to suffer a fatal case of COVID-19, the 60 and 70 year-olds, people are only 70% as likely to die of COVID-19 as they are to die of other causes in the course of a year. In addition, some fraction of those “normal” deaths will only have been hastened by COVID-19, so that the increased deaths in 2020 due to the coronavirus epidemic will actually be somewhat less. The exact fraction is hard to estimate, but since it is well-demonstrated that underlying poor health greatly increases the COVID-19 mortality, the number of older people whose deaths are only shortened by some months due to coronavirus is likely to be appreciable.
The fraction of life-years lost takes the life-expectancy of each age group into account, so that the lower COVID-19 mortality of younger people can be weighed by the larger number of years they would otherwise expect to live. From this, one sees that those 60-79 years of age will still lose the most years of extra life.
Perhaps these latter considerations help put the COVID-19 epidemic into perspective. Several points remain clear:
1. Efforts to avoid overload of the healthcare system will prevent a significant number of excess deaths, plus untold suffering
2. Applying modest measures of social isolation which achieve R0 values greater than unity are not sustainable long-term, and provide only a temporary bridge to another approach
3. Even a great success in completely snuffing out COVID-19 within a country with a limited number of deaths, results in a very delicate situation where the epidemic can easily re-ignite without constant vigilance
4. Universal deployment of an effective vaccine is the only real solution to achieve victory in this global battle


Comments by Readers
David MacLeod
Apr 13, 2020Thanks for sharing. When was this piece written?
Larry Horowitz
Apr 13, 2020One thing I’ve never understood is the need for forced immunizations (“universal deployment of an effective vaccine”).
If the vaccines are so effective, then those who opt to be vaccinated will have innoculated themselves against the virus. Why would they care if others choose not to be vaccinated?
Larry Horowitz
Apr 13, 2020This April 9, 2020 article by Robert F. Kennedy, Jr., Chairman of the Children’s Health Defense, about mandatory vaccination may be of interest.
Gates’ Globalist Vaccine Agenda: A Win-Win for Pharma and Mandatory Vaccination
Michael Lilliquist
Apr 13, 2020First, accroding to Erika Lautenbach (head of Whatcom County Health Dept.) in her comments to the Bellingham City Council on April 13, the current local transmission rate based on Whatcom County cases is 0.8, that is, below one. Each new case is not always leading to another new case. This indicates that social isolation may be working for the moment.
Second, my assumtion is that the US strategy is to sustain Option 3 until Option 1 become available. We have prett much overwhelmend Option 4, but it may become viable again if Option 3 succeed. Nonethless, we are sittign ducks until we finally get Option 1 up and running.
As indicated, Option 3 and 4 leave us vulnerable, while Option 2 is inhumane and needlessly consigns people to suffering and possible death.
Abe Jacobson
Apr 14, 2020Addressing Michael Lilliquist’s first point: It’s very hard to estimate the transmission rate if the vast, vast majority of the county population has never been tested. In fact, the county website speaks of fewer than 1000 tests, or about one-half of one percent of the county population. The proportion of cases that may be symptomatic could be as low as 50-70% in adults, and even lower in young children. That is, 30-50% of the infected carrier adults are likely to be asymptomatic, and the majority of infected carrier children are likely to be asymptomatic.
In addition, there are many healthy folks who go through the COVID19 disease and recover nicely, but are never tested. (Yes, I know two…) So they never appear in the COVID-positive category kept by the County statistics.
Bottom line: there is no reasonable basis upon which to state that the R0 factor for our county is 0.8.
Steve Harris
Apr 14, 2020Abe, you’re spot on with your analysis. I agree 100%. The “rate” of new infections that are confirmed are entirely dependant on the number of tests being performed. I believe that we will learn that the number of persons in Whatcom Co and elsewhere around the country who have (or have had) the SARS-Cov-2 virus is many magnitudes greater that what is currently believed. That’s good news.
Dick Conoboy
Apr 15, 2020For David and Steve (note this is being posted by Dick Conoboy as there seems to be some technical issues with Dr. Kellogg responding directly)
“David, I wrote this piece on 10-apr, but none of the conclusions should be time-critical
Steve, In the absence of testing, I believe you can get a pretty good estimate of infections by taking deaths and dividing by 0.009 (deaths/infection). I have not followed Whatcom Co numbers, since I am rather far away.
Yours, Dick Kellogg”
Abe Jacobson
Apr 15, 2020Dick Kellogg’s point is well taken. County website this AM says there are 285 confirmed cases (that is, revealed by testing. There are also 25 deaths confirmed from CV19.
25./0.009 = 2778 implied cases out there. A factor of 10 higher than County’s reported “confirmed cases”. So much for estimating R0 from “confirmed cases”.
Dianne Foster
May 06, 2020I wonder if those being tested at the Skagit Command Center who are from Bellingham are being recorded in the Whatcom County numbers. I went down there Friday for a test, since I’m immunosuppressed and had a terrible cold, and my SCCA docs wanted me to get one. (it was negative, yay!). But to get one here at the Whatcom Command Center you need to meet more criteria, like a fever. I don’t know how many Whatcom folks went down to Skagit, but someone should have that data.